Health
Ghana taps Zipline to maintain supply chain resilience amid USAID disruption

In the wake of ongoing disruptions to USAID’s supply chain, the Government of Ghana has partnered with Zipline, the world’s largest autonomous logistics system, to ensure uninterrupted access to essential health commodities, without adding a cedi to government spending. By leveraging Zipline’s existing network of autonomous drone delivery hubs, the government is reaching more patients than ever before while eliminating duplicative expenses long incurred by USAID.
In response to the recent stop-work order and the extended review of all USAID-funded programs, Ghanaian health authorities have swiftly prioritised the delivery of critical medical supplies through Zipline’s on-demand system. This includes a specific focus on malaria testing and treatment, which is critical amid growing concerns about the impact of climate change, including excessive rainfall and changes in weather patterns, which exacerbate the spread of malaria. Additionally included are medications for pain relief, cough, parasitic worms, and nutritional deficiencies. Each Zipline distribution hub is capable of hundreds of autonomous drone flights per day, providing the government with ample flexibility to absorb and deliver supplies currently sitting in warehouses across the country.
Zipline is supporting the delivery of these commodities across the Northeast, Northern, and Eastern Regions, with discussions underway to expand support to other parts of the country. Its rapid response to emerging needs across the health system enabled Zipline to scale deliveries at its various hubs by 20–50% in the last two months alone. Rather than navigating complex supply planning or rerouting, Regional Medical Stores centralised more products with Zipline, allowing on-demand deliveries to any patient, anywhere. By leveraging this flexible capacity, the government has significantly increased distribution volumes at no additional cost, while enabling system-wide savings by eliminating redundant logistics.
Commenting on the partnership, Comfort Addai Fofie, staff midwife, Jadema Health Centre, Northeast Region, remarked, “Zipline’s support in delivering essential medical supplies, including their recent delivery of some much-needed drugs to our facility, has been incredibly helpful in enabling us to discharge our duties effectively. Their timely deliveries and excellent collaboration have made a significant impact on our work. We’re truly grateful to the team for their continued efforts, they mean a lot to us in our line of duty”.
Daniel Kwaku Merki, Head of Zipline Ghana, said, “Ghana’s proactive approach to mobilising domestic resources and embracing innovative delivery solutions exemplifies its commitment to building a robust health system. This continued collaboration with Zipline is a clear example of how Ghana is transforming a challenging situation into an opportunity to build a more self-reliant and cost-effective health system – one that ensures critical care reaches every corner of the nation.”
By consolidating deliveries under Zipline’s existing partnership, which the government funds through a flat monthly fee for unlimited deliveries, Ghana can maximise its healthcare investments and ensure medical products reach communities more efficiently. This unified approach strengthens the nation’s health infrastructure, reinforces the Mahama Administration’s vision for economic growth and development, and ultimately delivers greater value for Ghanaian taxpayers.
Health
Revolutionizing Hospital Pharmacies: MedPharma’s COO on Financing, Efficiency and the Future of Drug Access in Nigeria

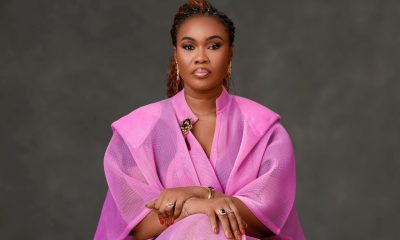
Yewande Adekoya is a Pharmacist and Healthcare Executive, currently serving as Chief Operating Officer/Head of Business at Medbury Pharmaceuticals. With over a decade of experience in business development, pharmacy management, and supply chain optimization, she has led strategic initiatives to enhance access to medicines, improve pharmaceutical care, and drive operational efficiency across Africa’s healthcare sector. At Medbury, she focuses on optimizing pharmacy and supply chain operations, reducing lost sales, and ensuring cost-effective access to quality medicines. Beyond her corporate leadership, Yewande has been instrumental in launching health-tech solutions, structuring mergers, and securing strategic partnerships to expand healthcare accessibility. In this exclusive interview with Alaba Ayinuola of Business Africa Online (BAO), Yewande speaks on MedPharma and its stock-financing model, quality assurance management, scaling MedPharma, and much more. Excerpts.
Alaba: What is MedPharma, and what inspired the creation of this model?
Yewande: MedPharma is a healthcare solutions company that provides pharmaceutical stock-financing for hospitals and healthcare providers in Nigeria. Our model addresses one of the biggest challenges in the healthcare system: lack of consistent access to essential medicines due to budget constraints. We were inspired by a simple question — What if hospitals never had to worry about upfront capital to stock their pharmacies? That question led us to create a model where we finance, stock, and manage hospital pharmacies entirely — with no upfront cost and no operational risk to the hospital.
Alaba: How exactly does MedPharma’s stock-financing model work for hospitals?
Yewande: Our model is simple but powerful. We finance 100% of the drug inventory and embed our operations team into the hospital pharmacy. This includes certified pharmacists, inventory software, and full logistics. We absorb all operational risk, manage procurement and distribution, and even return unsold or expired stock. Hospitals only pay once medicines are dispensed — and even better, they share in the profits. So, they earn revenue without tying up precious capital.
Alaba: What makes your model different from the traditional Drug Revolving Fund (DRF) system used in public hospitals?
Yewande: The DRF system requires hospitals to raise capital upfront, often from already overstretched budgets. It also exposes them to risks like stock expiry, theft, and poor forecasting. MedPharma’s model eliminates all of that. There’s zero upfront cost, no risk of dead stock, and our systems are built for transparency and efficiency. Think of us as a Public–Private Partnership (PPP) – we bring financing and expertise; hospitals retain control and benefit from consistent drug availability.
Alaba: How do you respond to concerns that outsourcing pharmacy operations may reduce transparency or hospital control?
Yewande: That’s actually a common myth. In reality, MedPharma operates strictly under hospital-approved Standard Operating Procedures. Pricing, formulary, and reporting structures are all jointly agreed upon with hospital management. Every transaction is digitally tracked, and weekly reports are shared transparently. The hospital retains full control, while we take on the heavy lifting behind the scenes.
Also, our model goes beyond end-to-end pharmacy management. A core strength of ours is supply chain optimization. Here, we streamline your backend operations covering inventory management, technology integration, and demand planning while you remain in charge of the front-end dispensary operations and patient interface. In this capacity, we can even serve as your silent, hidden partners, driving efficiency without disrupting your visibility or control.
Alaba: What results have your hospital partners seen so far?
Yewande: The impact has been remarkable. One partner hospital reported a 60% increase in pharmacy revenue within just one quarter of adopting our model. Another achieved less than 1% stock-outs over a six-month period.
Through our Pharmacy Benefit Program, we consistently maintain a 98–100% fulfilment rate. Even when a prescription cannot be fulfilled on-site, it is delivered directly to patients’ homes at no extra cost to the patient or the hospital.
For hospitals, this model has freed up significant capital. Funds once tied up in drug procurement have been reallocated to lab upgrades, staff training, and other critical investments.
For patients, the results are equally tangible: fewer delays, more prescriptions filled, and renewed trust in the healthcare system.
Alaba: How do you manage quality assurance, especially in a country where counterfeit drugs are still a major problem?
Yewande: As an ISO-certified company, quality control is at the core of our operations. All medicines we supply are NAFDAC-approved and WHO-certified generics or trusted brands, sourced directly from registered manufacturers. To further safeguard quality, we conduct periodic laboratory audits and independent batch testing. Our supply chain is deliberately structured to eliminate middlemen — reducing costs while also minimizing the risk of counterfeit products entering the system.
Alaba: What’s the most rewarding part of your work at MedPharma?
Yewande: For me, it’s walking into a hospital and seeing a fully stocked pharmacy, knowing that patients will get the care they need without delay. Or hearing from a hospital director who tells us they now have breathing room in their budget for the first time in years. We’re not just solving a logistics problem — we’re restoring dignity and efficiency to healthcare delivery.
Alaba: What’s next for MedPharma — are there plans to scale further?
Yewande: Absolutely. We are currently expanding our footprint across Nigeria and plan to onboard more state and federal facilities before the end of the year. We’re also investing in advanced inventory tech and analytics to further optimize drug availability. Our vision is bold: no hospital in Nigeria should ever experience a drug stock-out again — and we’re building the infrastructure to make that a reality.
Health
Emergency Care in Nigeria: Insights from Emergency Response Africa’s Inaugural Prehospital Emergency Care Stakeholder Summit.

In Nigeria, obtaining emergency medical assistance is a scarce privilege. There are only 0.4 ambulances available per 100,000 people, far below the WHO’s recommendation of one per 10,000. The stakes are exceptionally high for pregnant women and newborns, as more than 80% of maternal deaths in Nigeria could be avoided with timely intervention. It is against this stark reality that Emergency Response Africa (ERA) convened the inaugural Prehospital Emergency Care Stakeholder Summit, Beyond the Ambulance, in Lagos.
Inside the Four Points by Sheraton, healthcare executives, policymakers, emergency responders, and industry experts, recently gathered to address critical challenges in emergency care and explore solutions for a more efficient and responsive emergency care system in Nigeria.
The summit opened with a sense of urgency. “We cannot continue to treat emergency medical services as an afterthought in healthcare planning,” said Folake Owodunni, CEO of Emergency Response Africa. “Every second counts in an emergency and it is essential to create an ecosystem that ensures people get help when they need it most. Folake strongly advocates that strengthening emergency medical services has the potential to drastically reduce preventable deaths and improve timely access to medical care, especially in emergencies.
Her words resonated deeply with Dr. Benjamin Wachira, founder of the Emergency Medicine Kenya Foundation, who delivered the keynote address. “Africa needs a prehospital care system that integrates community engagement with technology. By training community members as first responders and leveraging digital tools for rapid response coordination, we can improve emergency care accessibility and efficiency” Dr. Benjamin emphasized.
54% of mortalities we get from emergencies can be averted if they had had pre-hospital care. says Dr. Tomi Coker, Honourable Commissioner for Health in Ogun State.
Before now, the focus of emergency healthcare has been within the facility and not pre-hospital, so the importance of this summit is that we are now having a conversation around what happens to accident victims or any medical emergency before getting to the hospital. Dr Tomi Coker outlined Ogun State’s recent efforts to combat maternal and neonatal mortality through the launch of the Maternal and Newborn Mortality Reduction Innovation and Initiative (MAMII), emphasizing the government’s commitment to enhancing maternal and newborn survival rates.
In Lagos, the most populous city in Africa, Permanent Secretary of the State’s Ministry of Health, Dr Olusegun Ogboye, says the state is working towards an emergency response system where there are available ambulances to attend to victims anywhere between 15 and 30 minutes before taking them to the hospital. As a state, emergency response is something we have a lot of passion for, it’s a cause we have been pushing for the last 4 or 5 years, and it’s the reason we are contributing to the Pre-hospital care conversation.
Amina Zakhnouf, Investment Officer at the Fund for Innovation in Development (FID), echoed the call for financial backing at the Summit disclosing that FID is committed to funding scalable solutions that save lives. We’ve partnered with Emergency Response Africa for the last 18 months, as a primary funder, we are pleased to be able to help them test and experiment with this new model of emergency care services, within Edo state. “At FID, innovation is key to solving some of the world’s most pressing challenges, including poverty, inequality, and access to emergency medical services.
While the discussions at the summit were inspiring, the obstacles remain daunting. Nigeria’s emergency medical services face numerous barriers: an absence of centralized emergency numbers, the lack of paramedics as a recognized health worker cadre, and an underdeveloped reimbursement framework that leaves EMS financing in a precarious state.
The summit highlighted innovative approaches already making an impact. Community-Based First Responder (CBFR) models, where trained volunteers provide immediate aid to emergency victims before paramedics and an ambulance arrive at the scene.
As the summit drew to a close, one message was clear: the time for theoretical discussions was over. It’s time for action. Public-private partnerships must be strengthened, regulatory frameworks must be established, and most importantly, emergency care must be accessible to all Nigerians—whether in Lagos or the most remote villages across Nigeria.
Folake’s final remarks underscored the urgency: “Every moment we delay, lives are lost. We must build a system that ensures emergency medical services are not a privilege but a right. In the last 18 months, we have done quite a bit of work across 3 different states in Nigeria and we have learned a lot of lessons that we believe can hold value as Nigeria journeys towards increased access to pre-hospital emergency care”
Health
New Study Finds Zipline’s Drone Deliveries Reduce Maternal Deaths by 56.4%

A newly published study has highlighted the transformative impact of Zipline’s drone delivery system on healthcare in Ghana. In collaboration with the Ghana Health Service (GHS), the study analysed healthcare data from 191 health facilities in the Ashanti Region, including hospitals, health centres, and Community-based Health Planning Services (CHPS) compounds, between 2017 and 2022.
The findings reveal a direct link between reliable medical supply availability and improved health system utilisation, leading to a 56.4% reduction in maternal deaths at facilities served by Zipline compared to facilities not served by Zipline. By ensuring consistent access to critical medicines and supplies, Zipline’s drone deliveries caused more expectant mothers to seek antenatal care and deliver in health facilities under skilled supervision.
Using a mixed-method approach, GHS and Zipline researchers assessed how drone logistics affect maternal health outcomes, examining changes in healthcare providers’ and patients’ satisfaction, perceived quality of care, and overall experiences with drone logistics. They found that faster, more reliable treatment fostered greater confidence in the health system, driving a 19.9% increase in antenatal visits and a 25% rise in facility-based deliveries. Simply––more births now occur under skilled care, reducing complications and improving survival rates. This surge in facility-based childbirths and timely emergency interventions contributed to the significant reduction in maternal mortality observed.
The study also found that the availability of critical medications including blood products, oxytocin, and anti-snake venom improved significantly, reducing stockouts that previously led to unnecessary referrals and delays in emergency care. Before Zipline’s intervention, healthcare facilities in the Ashanti Region faced frequent shortages of essential medicines, delaying emergency treatments and increasing maternal and neonatal complications. By ensuring that medical supplies were consistently stocked, Zipline’s drone delivery system played a crucial role in addressing these persistent challenges.
Both patients and healthcare providers reported significant improvements in healthcare delivery. With better access to essential medicines and supplies, facilities could treat more patients effectively, reducing unnecessary referrals and improving overall care efficiency. Healthcare providers noted that faster, more reliable treatment strengthened emergency response capacity, particularly for obstetric and neonatal cases, and increased patient trust in the system. As a result, more people sought care earlier, reducing complications and the need for urgent hospital transfers. Additionally, reduced transportation costs and time savings for healthcare workers contributed to overall cost efficiencies within the health system.
Ghana’s strategic approach to healthcare logistics has reinforced the resilience of its health supply chains. By integrating drone-enabled medical deliveries nationwide, the government has ensured that critical medicines reach hospitals, health centres, and CHPS compounds within minutes, preventing stockouts, improving health outcomes, and increasing patient confidence in the health system. The study’s findings highlight the country’s commitment to leveraging technology to bridge gaps in healthcare access, particularly in remote and underserved communities.
“These results demonstrate Ghana’s commitment to enhancing healthcare access and delivery through technology and innovation,” said Mrs Susana Nkrumah Ghana Health Service (GHS) District Director of Health Services for Sekyere Central. “By collaborating with partners like Zipline, we are ensuring that all Ghanaians, regardless of their location, receive timely medical assistance.”
The study’s release comes as global supply chain disruptions raise concerns about the availability of essential medical commodities and whether African governments can effectively navigate these challenges. Ghana’s proactive investment in logistics infrastructure, including its partnership with Zipline, has proven to be a strategic decision helping to mitigate disruptions, maintain reliable access to medical supplies, and strengthen public confidence in the healthcare system.
“The ability to move medical supplies efficiently has never been more important,” said Daniel Kwaku Merki, Head of Zipline Ghana. “By ensuring essential medicines reach healthcare facilities on time, Zipline continues to support the government in strengthening public confidence in the health system. This ensures citizens trust their access to life-saving preventative care and treatments, despite global supply chain challenges
The full research study is now available for download: A mixed method impact assessment of the use of aerial logistics to improve maternal health and emergencies outcomes in the Ashanti Region of Ghana.
-

 Oil and Gas2 days ago
Oil and Gas2 days agoTotalEnergies, Chevron Push for Faster Permits, Better Seismic Data in Africa
-
 Afripreneur11 hours ago
Afripreneur11 hours agoRevolutionizing Cross-Border Payments in Africa: An Exclusive Interview with Onyinye Olisah
-

 Energy2 days ago
Energy2 days agoUnited States (U.S.) Political Will, African Reforms Signal New Era for Energy Investment











