Health
Universal Health Coverage: Local action driving universal achievements

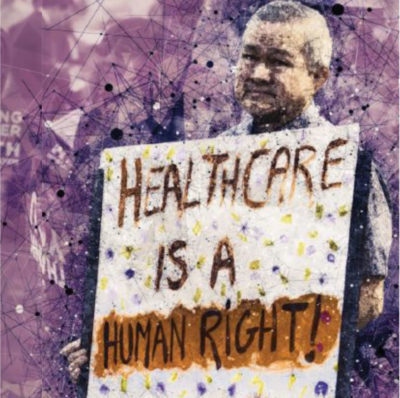
The world has never been as aligned on a common global health priority as it is now on universal health coverage. It is a global imperative for cohesive societies and economic prosperity. A consensus has existed since 1948 that health is a human right, and the call for health for all has been a lingering voice since 1978 at Alma-Ata. But there has never been such high advocacy as there is today with the current call for universal health coverage with access to essential services for all without financial hardship.
The United Nations High Level Meeting on 23 September 2019 in New York may be the climax of this building advocacy. Despite this celebratory moment, there remains a real fear that the political endorsements, high fives, dinners and numerous side events, will bring little change for half of the world’s population, living in Malawi, Vietnam, Somalia and other countries. This includes large numbers of people living in developed countries such as the United States who still do not have full coverage for essential health services.
As the world converges in New York this September, many issues will need to be prioritised. The UHC2030 movement, through its various multi stakeholder constituencies and wide-ranging consultations, has identified six key areas of focus. They start with political leadership beyond health and commitment to health as a social contract. Health is the foundation for people, communities and economies to reach their full potential – and the achievement of universal health coverage is primarily the responsibility of governments.
Governments ensure that people’s health is a social contract, noting that achieving universal health coverage is essential for inclusive development, prosperity and fairness. It requires political decisions that go beyond the health sector.
Second, half the world’s population is left behind. That includes the poor, migrants, criminalised populations and women. Health is enshrined as a fundamental right of every human being. Universal health coverage is key to reducing poverty and promoting equity and social cohesion.
Extending geographic coverage and reaching the most marginalised and hard-to-reach populations are essential to achieving positive health outcomes. For real action in all communities, governments must commit to report disaggregated data for the official statistics compiled on the Sustainable Development Goals in order to capture the full spectrum of the equity dimensions of universal health coverage.
The third priority is to ensure that governments create a strong, enabling, regulatory and legal environment that responds to people’s needs and builds institutional capacity, so the rights of people and their needs are met. There is no debating the fact that governments bear this primary duty under the International Covenant on Economic, Social and Cultural Rights.
The fourth call is to uphold the quality of care by building health systems that people and communities trust. That starts with primary health care as the backbone of universal health coverage. It is best achieved through creating confidence in public health systems that respond to people’s needs and deliver desired outcomes.Where private health services are required, leadership should come from the public sector.
The fifth call is for leadership through public financing and efficiency by investing more and investing better through sustainable public financing and by harmonising health investments from all players including development assistance and the private sector. Governments must adopt ambitious investment goals for universal health coverage and make progress in mobilising domestic pooled funding towards existing targets, such as 5% of gross domestic product or the African Union’s Abuja Declaration of 15% of government expenditure. This funding should be equitable and driven by the need to reduce impoverishing and catastrophic out-of-pocket expenditures for communities.
Furthermore, development assistance for health should reduce fragmentation and strengthen national capacities for health financing.
Finally, and in line with SDG 17 on the need for partnerships – and in recognition of the fact that health can only be achieved by a whole-of-society approach – countries should take active steps to engage non-state actors more meaningfully. In providing clear direction from the public sector, civil society and the private sector, they too can shape the universal health coverage agenda.
As in many other sectors, there is no one-size-fits-all answer. Solutions for each country must be tailored to that country’s particular context and population needs. The international community and global health partners should unite to support all countries to build a healthier world. The UN High Level Meeting in September must therefore reach high enough to mobilise political leadership but local enough to drive meaningful country action.
Githinji Gitahi joined Amref Health Africa as the group chief executive officer in June 2015. He is also a member of the Private Sector Advisory Board of Africa CDC, the Global Health Investment Advisory Board, and of the World Health Organization’s Community Health Worker Hub. Gitahi is co-chair of the UHC2030 Steering Committee, a global World Bank and World Health Organization initiative for universal health coverage. Gitahi has a doctor of medicine degree from the University of Nairobi and a master’s in business administration from United States International University.
Health
Remedial Health unveils new app with digital POS and barcode scanner

Remedial Health, a health tech startup that develops solutions to make Africa’s pharmaceutical value chain more efficient has unveiled an updated version of its customer-facing app, designed to function as an operating system for neighbourhood pharmacies and Proprietary Patent Medicine Vendors (PPMVs) across the continent.
The new app comes with a digital POS terminal to support payment collection, virtual business accounts to receive payments, an in-built barcode scanner feature for recording product sales and store-switch functionality to enable the seamless management of multiple stores, as well as inventory management solutions for restocking and easily identifying short-dated products. The app also offers comprehensive financial reporting to manage profit and loss, and data analytics to inform decision making.
Despite accounting for 85 per cent of retail medicines sold in Africa’s pharmaceutical industry (projected to reach $70 billion market size by 2030), the absence of bespoke digital tools to manage their unique sales and inventory management needs means neighbourhood pharmacies and Proprietary patent Medicine Vendors (PPMVs) are unable to run their operations as effectively and profitably as possible. At the same time, the reliance on paper-based inventory and sales management processes means manufacturers have limited empirical insights into customer behaviour to inform their decisions on production and distribution.
The new Remedial Health app has been designed specifically for healthcare businesses in Africa, with tailored features that have been designed to support effective decision making to drive business growth and profitability. Starting in Nigeria, healthcare businesses can access vetted medicines, and manage their sales and inventory on one easy-to-use platform, freeing up time and capacity to effectively serve their customers and communities. The app also enables Remedial Health to provide consolidated, real-time data on market behaviour to manufacturers for increased profitability and better decision-making across the value chain.
According to Samuel Okwuada, CEO, and co-founder of Remedial Health, “Neighbourhood pharmacies and PPMVs represent the frontline of healthcare delivery in Africa but they have historically been left to their own devices to figure out how to be efficient and profitable. Our mission is to empower these essential service providers with the tools they need to manage day-to-day operations and seamlessly run their practices effectively. We spent a lot of time interacting with our customers in the process of delivering this product and the feedback has been great. We are excited by the opportunity to get the app into the hands of pharmacies and PPMVs across the country to support their ongoing success, as well as the health and wellbeing of the nation”.
In 2023, Remedial Health sold more than 300 million individual packs of medicines to 7,500 hospitals, neighbourhood pharmacies and PPMVs across all 36 states of Nigeria. Its customers also improved their profits by 30 per cent on average, with access to more than 8,000 vetted products at the same, or better than, open-air medicine market prices. They can also access same-day delivery and leverage inventory financing to minimise cash-flow friction for routine orders and maximise sales opportunities.
Health
World Health Day 2024: Nurturing Health Through Nutrition

World Health Day (Family Photo)
As we commemorate World Health Day 2024 themed ‘My health, my right,’ the focus turns to the critical importance of good food and nutrition, particularly in regions like Central and West Africa. Nutrition is the foundation of human health, influencing every aspect of physical, cognitive, and emotional well-being. In these regions, where socio-economic gaps, environmental challenges, and diverse cultural norms converge, the importance of good nutrition becomes even more pronounced.
That is why multinationals like Nestlé are championing affordable and good nutrition for families through its brands while ensuring the sustainable sourcing of raw materials such as coffee, cocoa, soya among other ingredients in its supply chain.
“Nestlé reaffirms its commitment to promoting quality and affordable nutrition, particularly in Central and West Africa. We believe that access to balanced diets, rich in essential nutrients, is vital for maintaining optimal health and well-being. Together, we strive for a future where everyone has access to nutritious diets, ensuring not only physical health but also fostering local communities and prosperous societies,” says Mauricio Alarcón, CEO Nestlé Central and West Africa.
Foundation of Health
In Central and West Africa, numerous health challenges persist, ranging from enduring malnutrition to the rising incidence of diet-related non-communicable diseases. These nutritional deficiencies not only hinder physical growth and development but also weaken immune function, cognitive abilities, and overall disease resilience.
Essential nutrients found in a balanced diet, including vitamins, minerals, proteins, carbohydrates, and fats, are the building blocks of health. Ensuring adequate nutrition during critical life stages, such as pregnancy, infancy, and early childhood, is vital for optimal growth, development, and long-term health outcomes.
Preventing Non-Communicable Diseases
In recent years, Africa has seen an increase in the rate of non-communicable diseases such as diabetes, cardiovascular disease, high blood pressure, and obesity. This rise mirrors global trends but is amplified by unique regional dynamics. While infectious diseases remain significant, lifestyle factors, like diet and physical activity, drive much of this burden.
A balanced diet is paramount in promoting overall health and preventing chronic diseases. A balanced diet encompasses a diverse range of nutrient-rich foods from all food groups, including fruits, vegetables, whole grains, lean proteins, and healthy fats. This dietary approach not only supports physical well-being but also aids in weight management and reduces the risk of obesity and associated health issues.
Access to a diverse and balanced diet, rich in essential nutrients is not only a basic human necessity but also a prerequisite for achieving the UN Sustainable Development Goals (SDGs) related to health, well-being, and poverty alleviation.
Empowering Communities Through Education
Empowering communities through education on nutrition is a powerful tool in the fight against malnutrition. Providing knowledge about healthy eating habits and balanced diets through initiatives in schools, community centers, and healthcare facilities can help dispel myths and empower people to make informed dietary choices.
Fortified Essentials for Balanced Nutrition
Some companies, like Nestlé, recognizes the importance of nutrition and quality in their product offerings. For instance, Nestlé’s R&D center in Côte d’Ivoire employs scientists and food technologists dedicated to developing affordable nutrition solutions for the region. They consider local dietary preferences and nutritional needs, integrating regionally sourced cereals and plant protein sources into formulations. These products are fortified with essential micronutrients like iron, iodine, zinc, and other vitamins and minerals ensuring optimal nutritional value.
Additionally, these experts have access to Nestlé’s global network of experts, advanced analytical equipment, labs, and pilot plants across all company R&D locations.
Products like Maggi, widely recognized across the continent, are fortified with essential micronutrients such as iron and iodine, meeting local preferences while boosting nutritional intake. Likewise, Cerelac, enriched with iron, and Nido, fortified with calcium, provide vital nutrients essential for children’s growth and development.
In Nigeria, the company recently introduced Nido Milk & Soya, a product that integrates locally sourced soybeans. This initiative offers a budget-friendly option for nutritious consumption, while providing healthy nutrition among consumers.
Harnessing the Power of Collaboration
The path to improved nutrition in Central and West Africa necessitates collaborative efforts across sectors and stakeholders. By partnering with governments, civil society organizations, academia, and the private sector, we can combine resources, expertise, and innovations to drive meaningful change in the region.
Nestlé reaffirms its commitment to being a force for good by tackling the root causes of malnutrition, advocating for food security policies, and empowering individuals and communities with knowledge and resources for informed dietary choices. This in the long term creates a future where everyone experiences the highest standard of health and well-being.
Health
AstraZeneca launches Africa Health Innovation Hub to increase access to healthcare

AstraZeneca, a leading global pharmaceutical company, launched the Africa Health Innovation Hub today. This ground-breaking initiative highlights the company’s commitment to healthcare equity and fostering partnerships with a range of stakeholders, including governments, healthcare societies, academia, healthcare providers and patient advocacy groups, to better improve patient outcomes. Building on AstraZeneca’s work in Africa, the hub aims to use the latest science and technology to improve access to healthcare for patients on the continent.
The Africa Health Innovation Hub is the latest in the global A. Catalyst Network, a connected array of over 20 hubs worldwide. This network seeks to tackle current healthcare challenges through collaborative innovation, promote affordable and equitable healthcare access, and amplify patient-centred innovation through strategic alliances within the healthcare ecosystem.
Last year, AstraZeneca joined the WEF Edison Alliance, a public-private partnership that aims to improve the lives of 1 billion people through digital inclusion by 2025. The partnership reinforces our commitment to harnessing digital innovation to drive inclusion and equity across the healthcare ecosystem, therefore, will also be a strong facilitator of the Africa Hub.
Gagan Singh, Country President, African Cluster, AstraZeneca, stated, “AstraZeneca aims to strengthen and future-proof health systems across the whole patient journey, ensuring everyone has equitable and affordable access to the life-changing healthcare solutions they need, regardless of where they live. The launch of the Africa Health Innovation Hub is a significant step in our goal to unlock digital transformation and innovation in health across the continent, paving the way for patient-centric digital health solutions that leave no one behind. By working with partners across the continent, we are nurturing local talent and making quality health care more accessible for all.”
Partnering to bring our purpose to life
In Africa, two major new partnerships will form the backbone of the Hub in its initial phases:
- In South Africa, AstraZeneca is partnering with MEDSOL AI SOLUTIONS to help promote the use of AI in the detection of disease through a state-of-the-art Wi-Fi ultrasound probe that can detect breast cancer in seconds. The Melusi Breast AI rapid detection app will be rolled out in rural clinics to help in early detection of the disease, supported by a dedicated referral system so that women with positive detection of breast cancer can be offered a quicker turnaround time for therapeutic intervention.
Dr Kathryn Malherbe (PhD), CEO & Founder of MedSol AI Solutions said, “Medsol AI is excited to be leading one of the inaugural projects of the Africa Innovation Hub, with support from AstraZeneca. Breast cancer is a devastating disease, with many women in our communities only able to access late-stage diagnoses. The Melusi Breast AI project will enable us to leverage technology and innovation to improve early diagnostic detection rates and patient outcomes in local clinics, ultimately saving lives.”
- In Kenya, the company is expanding an already successful collaboration with Tricog Health Limited. After a few years of piloting an AI technology that connects ACS patients to health professionals and route them to the appropriate facilities, enabling early cardio-renal complications to be addressed in India, the African hub aims to enhance early diagnosis and treatment of Heart Failure using Tricog’s InstaECG AI tools for rapid diagnosis, reducing mortality rates and improving quality of life.

Dr. Charit Bhograj, CEO & Founder Tricog Health Limited added, “non-communicable diseases, including heart disease, are on the rise in Kenya and across Africa, and we know that the earlier these conditions are diagnosed, the better chance it is for patients to continue to live long healthy lives. By investing in digital health technology, the Africa Health Innovation Hub is enabling the use of advanced AI to screen and diagnose patients remotely, bringing high-quality health tools to people no matter where they live.”
Another partnership initiated last year and will officially form part of the Africa Health Innovation Hub is the Fuel Africa programme, launched by Futurize. This is the largest healthcare entrepreneurship programme on the continent, bringing together the brightest minds across universities in Sub-Saharan Africa to address some of Africa’s most pressing challenges in healthcare. For the second year in a row, AstraZeneca’s A. Catalyst Network partnered with Futurize to reinforce our strong commitment to fostering innovation in the continent by developing local talents.
Official kick off to AstraZeneca’s health innovation hub in Africa
The official launch event – which marked the launch of the hub and the kick off of the Medsol AI partnership – took place at the Daspoort Poli Clinic in Pretoria, South Africa, where healthcare practitioners were able to demonstrate the use of the Melusi Breast AI device in a community clinic setting, which is one of the first points of contact for clinical breast examinations and breast cancer screening for patients.
The Africa Health Innovation Hub will also invest in building local talent, promote policy change for cancer screening, close the gaps in healthcare access and improve the quality of life for patients in the African region, particularly in rural and underserved communities. These objectives are aligned with the four pillars of AstraZeneca’s A. Catalyst Network: Education and Awareness, Early Diagnosis and Referral, Connectivity and Technology, and Data Generation.




















